I’ve never written a diary.
Nope.
Never.
It’s not really me, is it?
I don’t need to write down my feelings. In fact I try to never have any…..
I don’t really have private thoughts. I tend to spew them about on social media.
However, I have decided to document the next chapter of the treatment of my foot issues on this blog.
Why?
Simple really.
At some point, someone about to start on daily IV antibiotics may stumble across this and it may have some information that helps them along their own journey.
I think of it as possible future peer support……
A short background to all of this.
A foot ulcer that has taken 10 months of treatment so far.
A fantastic team that tailor my care to my needs and life.
A list of old broken bones and trauma that I have no recollection of doing. Clearly alcohol must have been involved at some (or many) point……
So, this week I started the next chapter of this long and at times cheesy (its hard to wash a foot you have to keep dry) story. Before I was lucky enough to go to ADA in Orlando, myself and my team had agreed that the day after I got back I would start a 6-week course of daily IV antibiotics. That due to having to work away, I would be taught to self-administer these so as not to impact my life and importantly my income (no work, no money, no bills paid).
Day 1
Foot clinic first.
The ulcer was looking a bit worse for wear after a week on my feet and all that travel, but the general consensus was that it had fared well and the plan of self-care that we had agreed had worked in the main.
I was also fitted with a new offloading boot. Much more robust than the previous one and it will help aid the healing once the infections (yes, 3 to be exact) in my foot and bone have been banished. Of course, I look like a total knob! However, I managed that with ease even without foot issues so it’s not a problem.

Then, off I hobble to the Ambulatory Care Unit…..
First bit of good news was that they were expecting me and knew all about the need to self-administer.
Day 1 here was easy.
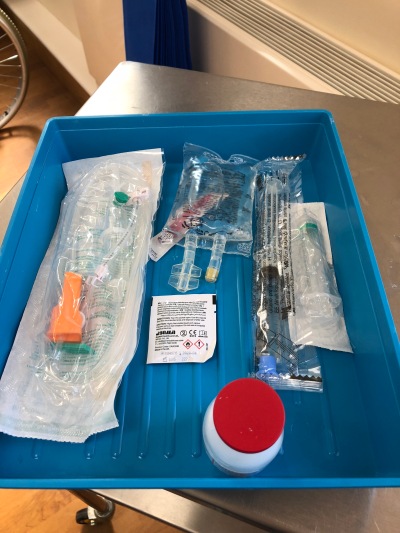
Cannula inserted.
IV drip set up.
30 min later I was on my way home to return on Day 2 for my first bit of instruction.
All that was left to do was to put on the new boot when home (you can’t drive in these things. To be honest you can barely walk in the bloody thing!), make a cup of coffee and over share the whole experience on Social Media…..
Day 2
Off I head to the hospital armed with a pad and pen!
Forcing myself to try and be a grown up always hurts but IV stuff is serious and whist I’m a dick head most of the time, this is the time to not be.
Today I was shown how to mix the antibiotics and set up the drip.
I wrote it all down step by step.
My writing is shit!
I mean, really shit.
So, had to take a bit of time to make sure I could read it later.
It’s a fairly simple process to be honest. The things I have had to do in the last 24 years that Diabetes has been living with me make it all easy to understand and there is no likelihood of me being overwhelmed with is because this just feels like and extension of what I already do….
My biggest challenge was actually to not tell myself “well that’s easy” and switch off my concentration.
With this going straight into my blood stream, I need to focus on infection control (because an infection whilst administering antibiotics for existing infections would really be taking the piss right now).
Anyway, there I am with 20 min on my hands as the drip is started.
Only one thing to do…..
Tweet it all out there…
I am very grateful for everyone’s best wishes that have been received.
For all that have voiced their concerns for me. I appreciate that too.
However, this is me, I am genuinely ok with this and this will have a successful outcome, and…..
You will have to endure endless tweets and posts about it too…
I am fully aware that my “resilience” can be my downfall. I am my own worst enemy at times as I push myself too far to prove to myself that I’m immortal. Not this time though. You don’t get rid of Grumps that easily…….
I’m back at the hospital again tomorrow, but will tell you about that, well, tomorrow.
Live Long and Bolus
Grumps.
Tags: #TalkAboutComplications, Complications, dBlog, Foot Care, Motivation, Type1